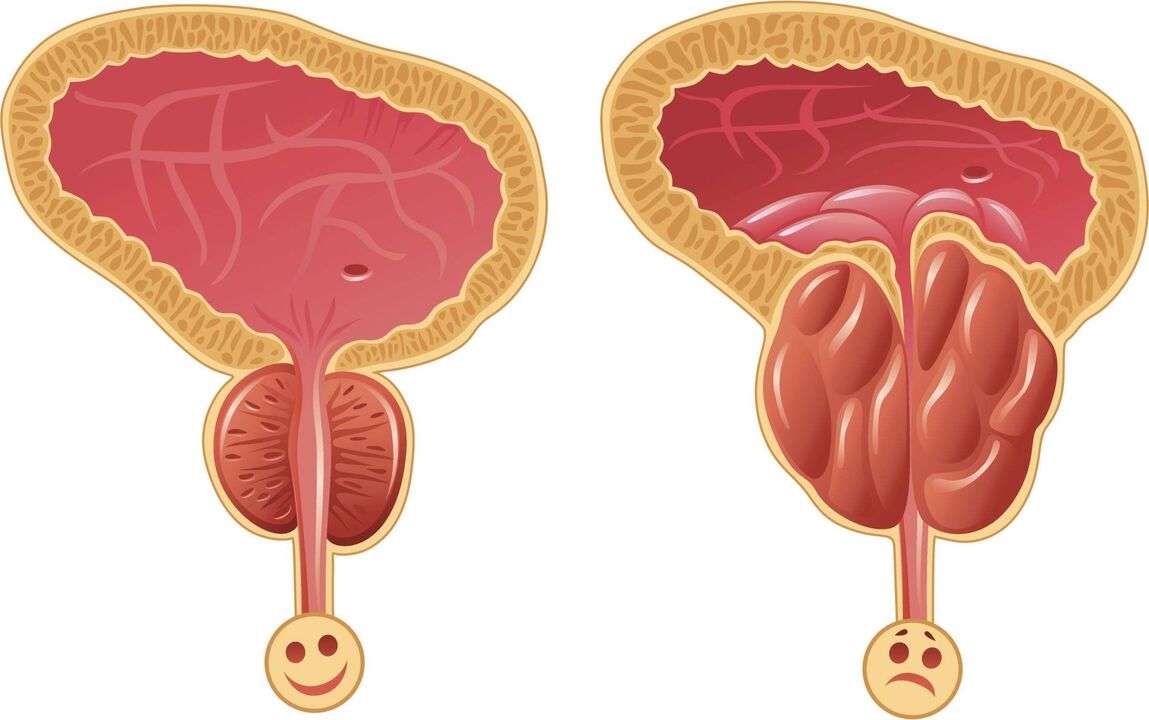
Inflammation of the prostate (prostatitis) is a very painful condition. But usually prostatitis is not limited to pain alone and causes even more serious symptoms. Which? How long does prostate inflammation usually last? And what helps from it?
What is prostatitis?
Prostatitis is inflammation of the prostate (prostate gland). The prostate can become inflamed as a result, for example, of bacteria that can enter the prostate tissue from the urinary tract. Depending on whether the cause of prostate inflammation is bacteria or not, the following types of prostatitis are distinguished:
- bacterial;
- abacterial prostatitis.
The prostate is a four-centimeter gland, which in men is located below the bladder. It is one of the internal reproductive organs that produces a secretion that mixes with sperm during ejaculation. This secretion provides sperm motility and provides support on the way to the female egg.
The prostate gland in men can become inflamed as a result of inflammation of the bladder or urethra (urethra), and the causative agents of inflammation can be bacteria migrating from the bladder or urethra to the prostate. In this case we talk about acute prostatitis. In most cases, the infection can be controlled with antibiotics.
In about 5 out of 100 patients, bacteria remain in the prostate despite treatment, leaving inflammation unchanged. Diagnosis of chronic prostatitis.
Bacteria are not always the cause of prostate inflammation
Besides bacteria, there are other factors that can cause prostate inflammation, such as central nervous system (CNS) disorders, mental problems, stress and chronic inflammation of the bladder wall. Since prostatitis in this case does not occur due to bacteria, it is called abacterial prostatitis.
Sometimes abacterial prostatitis is called one of the forms of chronic pelvic pain syndrome (CPPS for short). However, this pain syndrome can also develop without inflammation of the prostate. In addition to inflammatory, there are also non-inflammatory forms of chronic pelvic pain syndrome.
Note: In non-inflammatory chronic pelvic pain syndrome, the symptoms are similar to those of prostatitis, but neither bacteria nor signs of inflammation are found.
However, the official classification of prostatitis by the US National Institutes of Health includes both inflammatory and non-inflammatory forms of chronic pelvic pain syndrome.
According to many, this misleads doctors and, in the worst case, can lead to incorrect treatment. Unlike inflammation of the prostate gland, non-inflammatory chronic pelvic pain syndrome does not respond to antibiotic therapy.
Causes of prostatitis
There are a number of factors that contribute to inflammation of the prostate gland. The most important are:
- recurrent urinary tract infections;
- bladder catheterization;
- surgeries in the urogenital area;
- unprotected anal sex.
Under these and other circumstances, bacteria can easily enter the urinary tract and cause inflammation of the prostate gland. If bacteria enter the prostate, it can lead to bacterial prostatitis.
Abacterial prostatitis can have more diverse causes. Let's take a closer look at the causes of both types of prostatitis.
Bacterial prostate
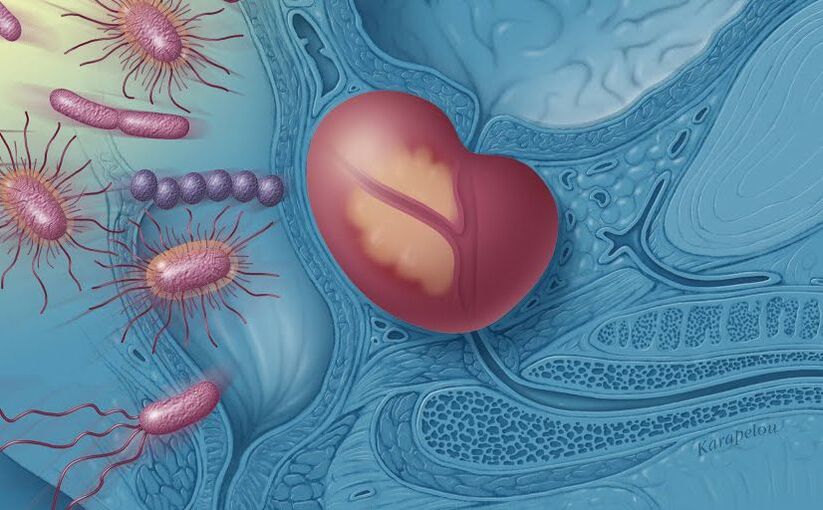
Most bacterial prostatitis is caused by intestinal bacteria such as Escherichia coli or enterococci. If they enter the urinary tract through the opening of the penis, they first cause an infection of the urethra or bladder, then the pathogens enter the prostate gland, causing inflammation of the prostate.
Men who get prostatitis in the hospital often have Pseudomonas aeruginosa. They enter the urinary tract after catheterization of the bladder.
In rare cases, prostate inflammation occurs as a result of sexually transmitted diseases. In this case, the causative agents are mainly chlamydia.
Abacterial prostatitis
In abacterial prostatitis (a form of chronic pelvic pain syndrome), any bacteria can be the culprit. However, after tests, leukocytes (white blood cells that protect the body) are found in the prostate and sperm. This indicates that the body is fighting inflammation.
What causes this inflammation is not fully understood and studied by specialists. This is likely the result of the combined effects of various factors. The following factors may play a role:
- impaired immune response;
- central nervous system disorders that affect the nerves and muscles of the genitourinary system and prevent a person from emptying their bladder as usual;
- mental disorders such as stress, anxiety or depression.
Some experts suggest that hidden infections may be the cause of chronic pelvic pain syndrome. However, this assumption is controversial.
Typical symptoms of prostatitis
Typical symptoms of acute bacterial prostatitis are:
- frequent urination;
- burning during urination (usually with a small amount of urine);
- pain in the bladder and perineum;
- pain during bowel movements;
- nausea, vomiting;
- fever and chills.
Chronic bacterial prostatitis also causes pain and problems with urination. However, these symptoms disappear immediately and then appear after a while. Chronic prostatitis is characterized by a recurrent course with fading and reappearing inflammation. It can last for many months.

Another characteristic sign of chronic inflammation of the prostate gland is erectile dysfunction.
Abacterial inflammation of the prostate, which is not caused by bacteria, essentially causes symptoms similar to those of chronic bacterial prostatitis. In addition, victims sometimes complain of pain during ejaculation.
Special case: asymptomatic inflammation of the prostate
In rare cases, the doctor may detect an increased number of white blood cells in the ejaculate or prostate secretions, but the affected person may not feel pain or other symptoms of prostate inflammation.
Such cases are classified as asymptomatic inflammation of the prostate and are usually discovered incidentally as part of a cancer or infertility screening.
Diagnostics
A doctor can diagnose acute bacterial prostatitis by asking the patient about his symptoms and examining the prostate. First, the doctor feels the prostate with his finger. If, upon palpation, warmth and swelling are felt in the prostate area, and the patient experiences pain, this indicates acute bacterial inflammation.
To confirm the diagnosis, the doctor may also do a urine test and draw blood from the patient to examine the level of inflammatory cells.
Chronic bacterial inflammation of the prostate cannot be diagnosed by palpation alone. For example, if the patient is between two bouts of inflammation, the doctor will not be able to detect severe swelling during palpation. Therefore, blood and urine tests are necessary to diagnose chronic bacterial prostatitis.
To detect chronic prostatitis, one urine sample is not enough. Because if the urine contains white blood cells and bacteria, this may also indicate a urinary tract infection. To find out if inflammation is affecting the prostate, your doctor will need to examine several urine samples.
Treatment of prostatitis
What treatment will help with prostate inflammation depends on the cause: if the inflammation was caused by bacteria, the therapy will differ from the treatment of abacterial prostatitis. However, in both cases, the doctor may prescribe anti-inflammatory drugs (so-called antiphlogistics).
Treatment of bacterial prostatitis
For bacterial inflammation of the prostate, antibiotics will help eliminate the symptoms.
- In case of mild acute prostatitis, the doctor must prescribe antibiotics from the fluoroquinolone group, the patient must take them for 10 days.
- If the inflammation is severe, the doctor may administer broad-spectrum antibiotics to the patient.
- If it is chronic inflammation, the patient usually takes a fluoroquinolone for 4-6 weeks.
Treatment of abacterial prostatitis
Doctors usually try to control nonbacterial inflammation of the prostate gland using a combination of different medications. For example, in addition to anti-inflammatory drugs, they may also prescribe what are called alpha-1 blockers. They relax the prostate and bladder muscles and thus promote bladder emptying.
Depending on your doctor's suspicions about the cause of the inflammation, further measures may be needed. For example, it has been suggested that psychological problems may also play a role in the development of nonbacterial prostatitis. In this case, the doctor may recommend psychotherapy.
In addition, thermal treatments such as baths can often be used to relieve symptoms.
Treatment of prostatitis with folk remedies
Folk remedies for prostatitis serve as an alternative to drug therapy. Used for bacterial prostatitis. Before using folk remedies, consult your doctor.
Fireweed
Fireweed has proven itself to be an excellent remedy for prostate diseases.

Fireweed is a perennial herbaceous plant. It has small, usually white flowers, but they also come in various shades of red.
Fireweed seeds are small; there is a fluff on their surface, with the help of which they spread.
There are about 200 species of fireweed, the plant is often regarded as a weed and can be very toxic, but beneficial effects have only been demonstrated in fireweed. Flowers and root are used. The content of biological active substances (myricetin, kaempferol, quercetin, lectin and sitosterol) has a positive effect on prostate activity.
Use of fireweed:
- Pour 1 heaping teaspoon of herb into 1/4 liter of water, bring to a boil and leave to brew for a short time (15 minutes). You should drink it in sips throughout the day (up to 2 cups) cool.
This medicinal plant is used for various urological diseases, in particular:
- for all prostate diseases, including prostate cancer;
- for kidney diseases;
- for diseases of the bladder;
- for bladder cancer;
- for wound healing.
Fireweed is effective against inflammation of the urological tract, as a rule, it is combined with other herbs, depending on the nature of the problems, most often with cranberry, goldenrod, horsetail or birch.
Green tea
Medicines in the form of green tea are probably the most pleasant way to treat prostatitis.
It is advisable to drink 3 cups of green tea per day.
This drink promotes frequent urination, which helps cleanse the entire body. In addition, green tea is directly involved in detoxifying the body.
Advice! Men are advised to urinate while sitting. In this way, complete emptying of the bladder is achieved. The sitting position thoroughly releases all the pelvic muscles, as a result of which no residual urine remains in the bladder, in which some pathogenic bacteria would otherwise quickly multiply.
Nettle
2 handfuls of freshly picked nettle leaves - about 15 cm from the top of the plant - should be poured with 300 ml of drinking water and left to infuse overnight (approximately 12 hours). In the morning, the infusion should be slightly warmed and drunk.
Cranberry
Cranberry is one of the famous fighters against prostatitis. Home treatment with cranberries involves consuming it in dried, fresh or canned form. In the latter case, however, you should beware of added sugar.

Cranberry juices are also available in stores. You should also be careful here and read the label carefully to ensure that the juice does not contain additional juices from other fruits or artificial sweeteners.
Only 100% cranberry juice has healing effects.
Add dried cranberries to porridge or oatmeal.
For whom cranberries are not suitable:
Cranberry is contraindicated for people taking blood thinning medications. Cranberry can reduce the antiplatelet effects of the drug, which will lead to bleeding.
Ginger
When treating prostatitis, you can pay attention to another useful product - ginger root. Ginger is a promising product for the treatment of this disease. It has a powerful anti-inflammatory effect and antioxidant properties, interrupts the reproductive cycle of cancer cells (which is especially important in the treatment of prostate cancer), and promotes apoptosis. Along with this, ginger is not toxic to other rapidly growing cells.
It should be taken after meals, adding the root to tea (preferably green).
Pumpkin seeds
As practice shows, the most effective method of treating prostatitis is to use fresh rather than dried pumpkin seeds.

Preparation: Pumpkin seeds should be crushed. The resulting mass is mixed with honey in equal proportions and slightly heated. Then you need to leave it in the refrigerator for several hours, after which you need to form balls the size of a walnut.
The balls are taken before meals, 1-2 times a day, daily.
For preventive purposes, you can eat 4-5 pumpkin seeds every day. They contain zinc, selenium and other biochemical substances that reduce inflammation in the body, including the prostate gland, and have a positive effect on the formation of the male hormone testosterone.
Chestnuts
Chestnuts are also effective and have no side effects, which is very important for older people.
The chestnuts should be peeled, crush the kernel into small pieces, pour boiling water over it and let it brew for an hour.
The decoction should be taken 3 times a day before meals, 30 drops.
Regular sex
Regular sex, just like masturbation, cleanses the prostate, promotes blood circulation, and prevents local inflammation.
Prognosis: duration and course of prostatitis
Acute prostatitis usually responds well to treatment. If the patient takes the antibiotics prescribed by the doctor, the pain and fever usually go away within 36 hours. After a few days, symptoms should decrease significantly.
Chronic prostatitis lasts several months and usually occurs in relapses, between which the patient experiences little or no discomfort. Chronic prostatitis is usually more persistent than acute prostatitis: antibiotic therapy often lasts several weeks.
Is it possible to prevent prostatitis?
Early treatment of urinary tract infections can prevent germs from spreading to the prostate and therefore prostate inflammation. Using condoms may also help prevent prostate inflammation caused by certain sexually transmitted diseases.
























